Orthobiologics
Orthobiologics in Orthopaedics
Mr Aslam Mohammed has extensive experience in treating patients using orthobiologic techniques this includes high-level athletes and those involved in sport at a recreational level. He has used orthobiologics in appropriate cases to help and treat specific soft tissue and joint conditions.
What are Orthobiologics?
Orthobiologics are number of treatment techniques available that help and enhance the normal healing process of damaged and injured tissues. This is a combination of concentrated cells and chemical molecules from the patient's own body, or it can be a manufactured product that is used.
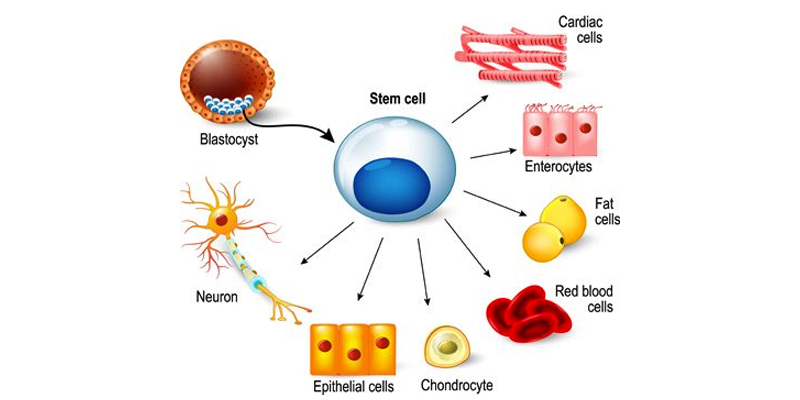
The cells can be mesenchymal stem cells (MSC) or cells are obtained from the patient, grown in the laboratory and then implanted back into the patient as in Autologous Chondrocyte Implantation (ACI) for articular cartilage damage.
There are a number of tissues in the body where MSCs can be obtained these include bone marrow, adipose tissue (fat) and peripheral blood.
The use of orthobiologics including Platelet-rich plasma (PRP) and Bone marrow aspirate concentrate (BMAC) in orthopaedic practice has increased significantly over recent years due to its autologous nature, supposed effectiveness and lack of side effects.
What different types of treatment are there?
Mr Aslam Mohammed uses following techniques in his practice:
• Platelet-rich plasma (PRP)
• Bone marrow aspirate concentrate (BMAC)
• Autologous Chondrocyte Implantation (ACI)
What is the evidence for their use?
PRP – It is not exactly clear how PRP works, laboratory studies have shown that the increased concentration of growth factors in PRP can potentially speed up or help the healing process.
Studies have evaluated the effectiveness of PRP treatments. At this time, the results of these studies are encouraging, but the effectiveness of PRP therapy can vary in individuals, further studies are on going.
There are many factors that can affect the outcome of PRP treatment these include:
• The area of the body being treated
• Degree of wear in the joint
• The general health of the patient
• The duration of the problem; an acute injury or chronic
• The Method of PRP preparation
• Application in injuries or after a surgical procedure
BMAC - The evidence situation is similar with on going studies comparing different treatments. The research into stem cells and arthritis shows is that stem cell treatment to be used as injection therapy alone and/or in addition to orthopaedic surgical procedures.
Successful stem cell therapies have resulted mostly in pain relief and improvement in function or quality of life.
Only a few limited early studies have demonstrated improvement in new cartilage or bone formation needed to cure arthritis.
Exactly how that cartilage regrowth occurs, or even how pain relief is achieved is not clear and the mechanisms are being studied. So at present the aims of the stem cell procedure, will be used to treat the symptoms of arthritis only. The ability to cure the disease entirely is not possible.
Who is suitable for this treatment?
Mr. Aslam Mohammed will assess your individual case and suitability for orthobiologics treatment, this depends the tissue or joint injury. For example in articular cartilage injury it will depend on the extent of the damage to the articular cartilage and the MRI scan findings along with a detailed history and examination.
What investigations are needed?
X ray with different views.
A high resolution MRI scan (Magnetic Resonance Imaging), which details the articular cartilage, soft tissues, meniscus, ligaments and bone marrow.
What does the procedure involve?
Click and See PRP
Click and See BMAC
Click and See ACI
What are the risks?
The risks are minimal as is you own blood and tissue being used in these treatments.
The possible risks will be discussed with you in detail before you make the decision have the treatment.
Platelet Rich Plasma (PRP)
Platelet rich plasma (PRP) has been used since the 1950s to manage maxillofacial and dermatological conditions, only recently has it come to be used in orthopaedics as adjunct to surgical procedures or as a specific treatment for soft tissue injuries and degenerative conditions.
Platelet rich plasma (PRP) is an autologous blood product with increased platelet concentrations. The process involves, taking blood from the patient, which is then centrifuged (spun at high speed) to obtain a concentrated suspension of platelets. PRP owes its therapeutic properties to the growth factors released by the platelets, which have regenerative and healing properties.
All PRP injections are not the same. The exact make-up of platelet-rich plasma depends on several variables, including the concentration of platelets, the concentration of white blood cells, and the use of additives.
Concentration of platelets in normal blood is 150,000 to 450,000 platelets per microlitre (μL), and the concentration of platelets in platelet-rich plasma can vary from 2.5 to 9 times that. The concentration levels depend on the individual's blood, how much blood was drawn, the centrifuge process (e.g., rotation speed and duration), and other clinical preparation methods.
The White blood cell count (WBC) also can effect the outcome in PRP treatment. The immune system depends on white blood cells to fight infection, but the cells' role in PRP therapy is unclear. Some experts suspect that white blood cells inhibit tissues' ability to heal, perhaps promoting inflammation, scar tissue, and damage to nearby tissues. Other experts think that, while white blood cells may not aid tissue healing, they have no negative effects, or may have beneficial effects. All this is being investigated at present.
In the knee, PRP has been utilised in patients with articular cartilage damage, ligamentous and meniscal injuries with variable success and outcomes.
There has been research conducted to evaluate the effectiveness of PRP in the treatment of the arthritic knee. This shows PRP can be of benefit in some patients who do not have bone on bone arthritis.
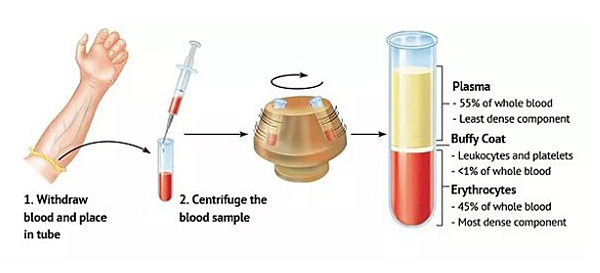
Principle of PRP preparation. Mr Aslam Mohammed uses the Arthex ACP system of preparation of PRP.
What are the functions of platelets?
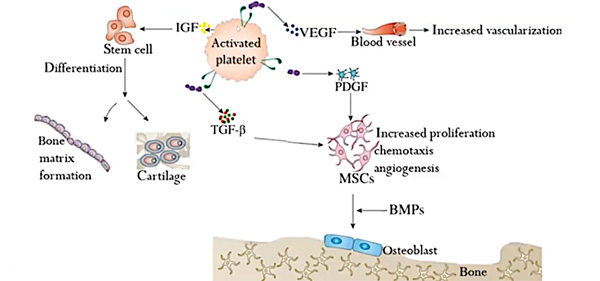
The efficacy of specific growth factors in healing various injuries and the concentrations found within PRP are the basis for the use of PRP to help tissue heal and repair. Platelets are key effector cells modulating haemostatic and inflammatory response activating other cells to release growth factors and cytokines.
Platelet function
Bone marrow aspirate concentrate (BMAC)
Initially described in 1952, bone marrow aspirate concentrate (BMAC).
This is obtained by aspiration of the bone marrow from the posterior iliac crest using a special needle to obtain approximately 60ml of bone marrow aspirate. This then spun at high speed in a centrifuge to concentrate the number of the MSCs, forming the BMAC.
The BMAC is then injected into the area of the body being treated. These MSCs have the potential to change into different types of tissues depending on the local environment and stimulating factors present. In doing so they may be able to repair and restore damaged tissues.
BMAC has been used in treatment of arthritis of the hip and knee to help regenerate the articular cartilage with variable results.
Stem cell potential to develop into different tissue types dependent on the environment and chemical stimuli.
- Orthobiologics in Orthopaedics
- PRP - Platelet Rich Plasma Therapy
- Cartilage Repair
- BMAC Bone Marrow Aspirate Concentrate
North West Hip & Knee Clinics
Services provided:
• Keyhole (minimally invasive)
• Hip and Knee Surgery
• Hip and Knee Joint Replacement
• Hip and Knee Sports Injury
• Hip Arthroscopy, FAI and Labral Surgery
• Knee Arthroscopy and ACL / PCL
• Ligament Reconstruction
• Biologics – PRP, Stem Cell
• Cartilage Regeneration
Mr Aslam Mohammed Consultant Hip and Knee Surgeon